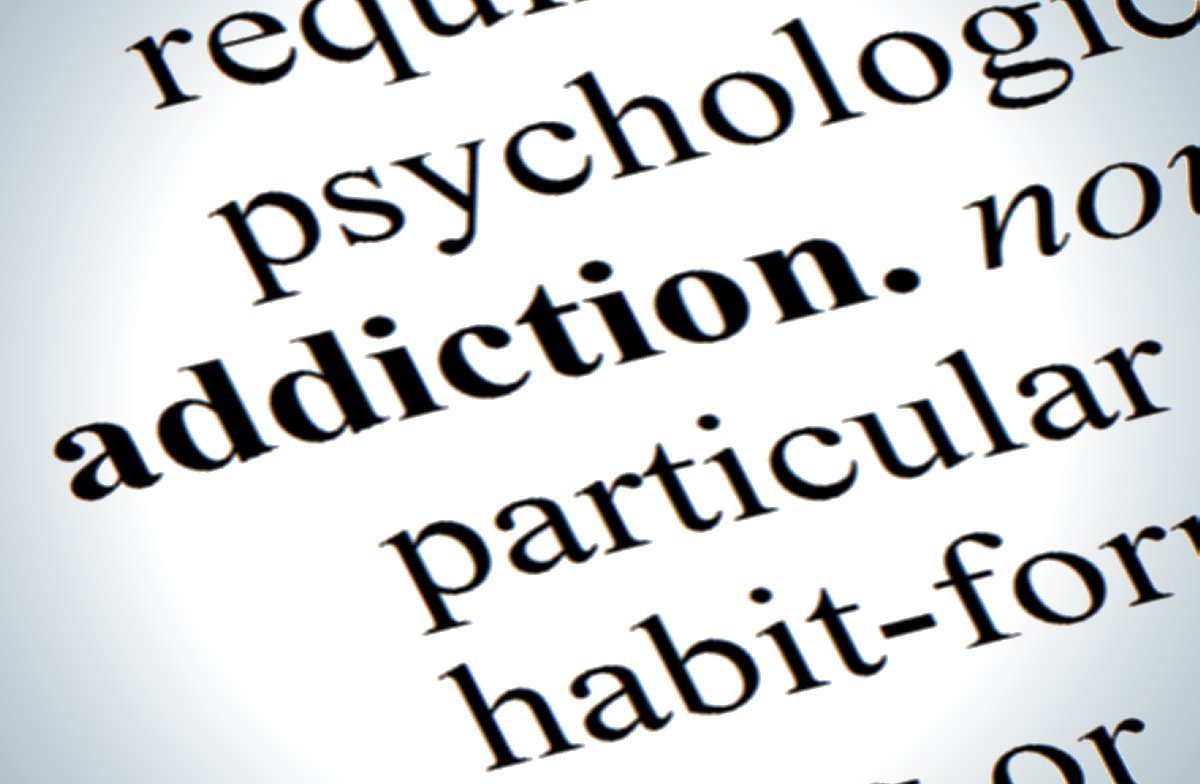
The United States is facing a major health crisis, and you may not have heard much about this one in the national news: according to the National Institutes of Heath, about 1 in 12 Americans abuse illicit drugs.
The Chicagoland area is no stranger to this issue – Chicago, and even some of its suburbs, face one of the largest drug abuse crises in the country. Illicit drug use can be dangerous by itself – even a single dose can be fatal – but for some individuals, casual drug use can almost naturally transition into a full-fledged substance abuse disorder, or addiction, without much thought. A substance abuse disorder is a brain disease where someone loses the ability to stop using drugs, despite its negative consequences on his or her physical, mental, social, and economic well-being. For individuals with substance abuse disorders, drug use becomes a compulsion, and it becomes extremely difficult to stop without help.
Despite these daunting circumstances, Chicago is fighting back. The city and surrounding areas are home to several drug and alcohol treatment centers, which have given individuals who struggle with substance use a second chance at living a normal life. These centers employ an army of psychologists and social workers who have dedicated their lives to caring for and treating individuals with drug and alcohol problems. One of these specialists is Ina Sherman, a recovering alcoholic herself, who is now a certified drug counselor at the Chapman Center in Evanston. Ina sat down with us to discuss her role in stopping addiction in its tracks and to discuss her own views on how addiction is treated today.
Can you tell us a little bit about where you work and what you do there?
I work at the Chapman Center at NorthShore University HealthSystem. My title is Certified Alcohol and Drug Counselor (CADC). The Chapman Center is an outpatient treatment center for patients who are dependent on mood-altering substances of all kinds. The population we serve is adults eighteen and older who are seeking a new way of life. They receive medical and psychiatric care, and participate in group and individual therapy to begin to address the underlying causes and conditions of behaviors and the symptoms of the disease. Every patient has a case manager who helps individualize care. There is also a family component to treatment that provides family counseling and education. Our program is medically based so each patient is evaluated and treated for co-occurring disorders, chronic pain, and other related health issues with special care given to supervising detoxification and medication management. We have a psychiatrist and nurses who see patients daily.
What degrees and/or certifications do you have that apply directly to your current job? What sort of training prepared you for this job?
I graduated with a degree in education from Northwestern University, taught for seven years and then worked in an unrelated field for most of my career. I returned to school in 2006 to begin classes that are required by the State of Illinois in order to receive certification for alcohol and drug counseling. I took a licensing exam, and every two years a CADC must take 40 hours of continuing education to be recertified. There is a licensing board that sets educational and ethical requirements.
Describe your typical work day.
My primary responsibility is to facilitate psycho-education in group settings. I teach seminars on a variety of subjects that are relevant to addiction and recovery. Topics range from learning about 12 step principles and participation to current information about brain science and the disease model of addiction. I facilitate groups on relapse prevention strategies, mindfulness, and goal setting. We try to build in experiential learning opportunities such as meditation, reflection, journaling etc. as well as connecting patients to the local 12 step meetings.
I often meet with patients individually to recommend 12 step meetings, to connect them to individuals in the program in their local communities, etc. Some patients just need extra encouragement and “recovery coaching” and I try to do a little of that.
Can you tell us a little bit about the patients you work with?

Relapse rates for drug addiction are similar to those of other common chronic illnesses. Therefore, addiction should be treated as if it were any other chronic illness. Source: JAMA, 284:1689-1695, 2000.
In general, our patients come because they want help. While we sometimes have court-mandated people in the program, all of our patients are motivated to get well. They are addicted to all kinds of substances – alcohol, street drugs and prescription medication. We believe that once you cross the line to addiction with one substance, you are addicted to all, so we treat them in integrated groups. Every patient must meet the criteria for addiction as described in the DSM*. They go through an assessment process, and some patients are recommended to a higher level of care, such as residential treatment. Alternatively, if it is determined that their primary diagnosis is something that we don’t focus on, such as eating disorders, we will help them find the right program. Most patients are in the early stage – some still on medical detox** when they begin. We also have people who are coming back into treatment after a relapse who need additional help. Most people who come into treatment are ambivalent at first, but through education and large doses of empathy and compassion, they come around to the notion that change and sobriety are actually possible.
Editor’s notes:
*The DSM (The Diagnostic and Statistical Manual of Mental Disorders) is the handbook that psychologists and psychiatrist used to define, categorize, and diagnose mental disorders. Since there are no accepted physiological tests for diagnosing mental disease (for instance, there is no blood test for drug dependence), medical professional rely on the psychosocial criteria listed in the DSM to diagnose mental disease.
**Medical detox is the process of clearing a drug from the body. When addicts first arrive at a hospital or treatment facility, there may still be a high concentration of drugs in their blood and tissues. In addicts, the body gets used to having these drugs in the body, and if they are suddenly removed, the patient might experience dangerous withdrawal effects. Therefore, detox must be handled very carefully by medical professionals. Detox involves slowly stepping down the concentration of drugs in the body so that the body can adjust gradually.
What has led individuals to come to your department? What happens after they leave your department?
People come to the Chapman Center through recommendation from people who have been through the program and through referrals of physicians, therapists and psychiatrists. We have been treating patients for over thirty years, and I am proud to say that we have an excellent reputation in the community. After primary treatment that lasts anywhere between five to seven weeks, many patients participate in an aftercare program which brings them back to the center once a week for twelve weeks. This keeps them connected to the help they need to get back into their lives or to create new ones. Some also continue to work with our psychiatrist.
What influenced you to pursue this path of work?
I am a recovering alcoholic with about fifteen years of sobriety. After leaving another career in 2006, I decided to go back to school with the idea that I would love to give back to the recovery community in a more meaningful way. Although I never dreamed that I would be hired at the age of 60 by what I thought was the best treatment center in my community – that in fact happened! I am grateful to serve this community. I feel blessed to have this opportunity to continue to learn about addiction and recovery strategies. It is my work and also my passion.
Are you involved with any counseling outreach in the community?
I write a monthly article about topics related to substance abuse for a community newsletter in Evanston. I have spoken at community meetings in the area about addiction and the impact it is having on the lives of individuals and communities. As a service project, I have had the chance to establish a weekly 12 step meeting at our center that draws from the general community, but in particular attracts Chapman Center alumni.
Amid the effort of stopping addiction, do you think that science and religion clash, complement each other, neither, or both?
 Since beginning to do this work, this question has been the focus of a great deal of my thinking and research. Many folks reject 12 step programs because they believe that they are religious and refuse to attend because they think that they are going to be forced into a particular set of beliefs. In my own experience, I have found that over time, one can come to develop their own spiritual values and practices.
Since beginning to do this work, this question has been the focus of a great deal of my thinking and research. Many folks reject 12 step programs because they believe that they are religious and refuse to attend because they think that they are going to be forced into a particular set of beliefs. In my own experience, I have found that over time, one can come to develop their own spiritual values and practices.
I try to help patients figure out where they stand on this issue and then find a place where they can enter 12 step program if they choose to – but with the attitude that they can “take what they want and leave the rest behind.” (An AA Slogan) I have come to see that science and spirituality often overlap. I try to guide patients to find the intersection of neuroscience, positive psychology and their own definition of spirituality, and then make an educated decision on how they want to move forward. Personally, I find that non-theistic Buddhist practices and neuroscience are very complementary and support the work of the 12 steps that includes self awareness through meditation and other daily practices, and a focus on the present moment.
And finally, I think that if Albert Einstein could say that either everything is a miracle or nothing is, I can accept that science and spirituality both accept mystery as part of any process of change.

An ad for Guinness beer from 1968.
What is your opinion on how drug addiction is perceived in society?
I believe that there is a deep paradox in our culture. We look upon use as acceptable – until it isn’t! College binge drinking, the glorification of drinking and using in movies and film, and the barrage of advertising let young people know that using is “normal.”
With the increase of prescriptions for pain relief, and depression and anxiety, many people come to believe that these medications must be safe. But once someone crosses the line to addiction, that person is often marginalized or seen as morally deficient or at least lacking in willpower. Addiction is an epidemic with tremendous costs to individuals, families and communities. However, recovery is possible – advances in treatment strategies, effective medication and neuroscience have contributed to the possibility of better outcomes. I wish BOTH parts of the message were being communicated.
Name one thing you would like to change about the way addiction treatment is conducted.
I think that treatment needs to be more universally available. And I would hope that more treatment centers would use the disease model as the basis for treatment as well as other modalities. If patients begin treatment with the idea that they have a disease and are not “bad,” they have a chance to move through the shame and get the help they need. Addiction is a chronic disease just like diabetes and arthritis, and it needs to be treated as such.
Ina’s recommendations for further reading:
There are several psychologists/scientists that have influenced my understanding of addiction:
I like Rick Hanson who wrote Buddha’s Brain. He makes neuroscience accessible to someone without a scientific background.
I use the work of Jon Kabat Zinn on mindfulness. Research is now demonstrating how the use of meditation techniques can positively impact health outcomes.
I believe Brene Brown’s work on shame and vulnerability is extremely influential as these two areas are particularly connected to addiction and recovery.
I also like to read the research coming from the University of California at Berkeley. The research that they present through their website validates many of the practices such as gratitude, journaling and meditation that people in addiction knew anecdotally worked for them.
-
Ben Marcus is a public relations specialist at CG Life and a co-editor-in-chief of Science Unsealed. He received his Ph.D. in neuroscience from the University of Chicago.
View all posts