In the summer of 2018, you probably heard the word “glioblastoma” popping up quite frequently in news reports upon the decline and death of American politician John McCain. McCain was diagnosed with the aggressive class of brain cancer in July 2017, stopped treatment on August 24, 2018 and passed away the very next day. While this timeline might seem exceptional, the unfortunate reality is that McCain’s experience with glioblastoma is a very accurate representation of the rapid progression of the disease. In fact, those afflicted by glioblastoma survive on average just over one year upon diagnosis. Let’s explore what makes glioblastoma so evasive in nature and what scientists are doing to try to increase patients’ lifespans.
What causes glioblastoma?
 Cell division is a natural and necessary process—it’s responsible for replenishing our hair and nails, healing the skin after a cut, growing the skeletal system as a child develops into an adult and many other biological functions. Cells typically exhibit a phenomenon known as a contact inhibition, which means that they stop dividing when they bump into other cells. In this way, contact inhibition prevents the accumulation of cells in places where we already have enough. But this system doesn’t always work as planned. In fact, glioblastoma occurs when cells in the brain undergo genetic adaptations that allow them to bypass contact inhibition and divide uncontrollably.
Cell division is a natural and necessary process—it’s responsible for replenishing our hair and nails, healing the skin after a cut, growing the skeletal system as a child develops into an adult and many other biological functions. Cells typically exhibit a phenomenon known as a contact inhibition, which means that they stop dividing when they bump into other cells. In this way, contact inhibition prevents the accumulation of cells in places where we already have enough. But this system doesn’t always work as planned. In fact, glioblastoma occurs when cells in the brain undergo genetic adaptations that allow them to bypass contact inhibition and divide uncontrollably.
This happens because the adaptations alter the amounts and activities of different proteins within the cell that regulate cell growth. For example, glioblastoma cells make more of the enzyme IDH1, which plays an important role in building cell membranes. Glioblastoma cells may also feature genetic mutations that hinder proteins that initiate the process of killing defective cells. By creating more of those proteins that enable cells to grow and survive and deactivating those that cause them to die, glioblastoma cells can proliferate unabated and ultimately form cancerous tumors.
But, you may be asking, “What causes these changes in the first place? Well, “What causes cancer?” is the million-dollar question, and these days it can seem like the answer is… everything. Although glioblastoma does not appear to be hereditary, researchers have discovered that rare genetic disorders that feature similar cell division-inducing abnormalities, such as Li-Fraumeni and neurofibromatosis, may predispose an individual to glioblastoma development. Additionally, scientists have found that glioblastoma risk is associated with exposure to anything that is proven to damage DNA, such as cigarette smoke, radiation, and toxic chemicals.
Why is glioblastoma so difficult to treat?
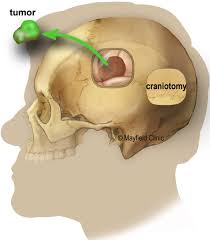
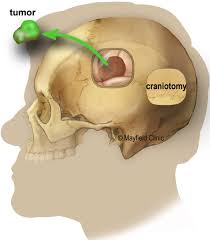 The fact that glioblastoma affects the brain makes treating it very complicated. A common first treatment step for any cancer is to remove tumors surgically. Surgery is a relatively straightforward process in other types of cancer, but removing a brain tumor presents a complex dilemma: If you don’t remove the entirety of the tumor, it will eventually reform, but if you are too generous in deciphering the tumor boundary, you will damage healthy tissue and risk causing permanent brain damage. For this reason, the vast majority of glioblastoma patients who undergo surgery relapse.
The fact that glioblastoma affects the brain makes treating it very complicated. A common first treatment step for any cancer is to remove tumors surgically. Surgery is a relatively straightforward process in other types of cancer, but removing a brain tumor presents a complex dilemma: If you don’t remove the entirety of the tumor, it will eventually reform, but if you are too generous in deciphering the tumor boundary, you will damage healthy tissue and risk causing permanent brain damage. For this reason, the vast majority of glioblastoma patients who undergo surgery relapse.
 The second widespread treatment option for cancer is chemotherapy. Glioblastoma patients typically receive chemotherapy in the form of the drug Temozolomide, which causes cancer cells’ DNA strands to break, triggering their death. But with time, glioblastoma cells manage to produce more of an enzyme that counteracts the drug and repairs the DNA, thereby enabling cells to survive. This issue of unprecedented resistance is the reason that glioblastoma is notoriously difficult to treat with chemotherapy.
The second widespread treatment option for cancer is chemotherapy. Glioblastoma patients typically receive chemotherapy in the form of the drug Temozolomide, which causes cancer cells’ DNA strands to break, triggering their death. But with time, glioblastoma cells manage to produce more of an enzyme that counteracts the drug and repairs the DNA, thereby enabling cells to survive. This issue of unprecedented resistance is the reason that glioblastoma is notoriously difficult to treat with chemotherapy.
What alternative treatments are scientists developing?
Scientists are currently developing treatments for glioblastoma that target those critical enzymes that cancer cells exploit in order to survive and thrive. One approach, called small-molecule inhibition, entails treating cells with a compound that binds to the mutated or overactive protein and shuts it down. The small-molecule inhibitor Ivosidenib, for example, recently became available to the public after extensive clinical trials. It binds to IDH1 to combat its role in helping cells to divide uncontrollably.
Alternatively, rather than impairing the activity of proteins that promote cell division, other experimental treatments seek to decrease the overall amount of such proteins in the cell through a process known as gene knockdown. This technique disrupts the normal way our genes serve as the instruction manual for building proteins in our cells. By inserting a certain DNA sequence into the cell, we can temporarily obscure the section of genetic code specific to one protein, making reading the manual (and therefore building the protein) impossible. This strategy can be used to reduce the level of production of proteins that stimulate cancerous growth.
Looking forward
The challenge of effectively treating glioblastoma has forced researchers to abandon the traditional approaches to other types of cancer and examine the disease from every possible angle. The commercialization of new small-molecule inhibitors and the currently developing research on gene knockdown agents marks a promising step toward improving the prognosis of those battling this merciless cancer. One day, thanks to the collaborative efforts and cumulative contributions of many scientists, health professionals and affected families, a glioblastoma diagnosis may no longer be synonymous with a death sentence.
 Sarah Anderson is a PhD candidate in the chemistry department at Northwestern University.
Sarah Anderson is a PhD candidate in the chemistry department at Northwestern University.
-
Sarah Anderson is a health, environment and science reporter at Northwestern University's Medill School of Journalism and a Ph.D. chemist. Follow her on Twitter @seanderson63.
View all posts